Joint strategic needs assessment
Self-harm (2019)
This is an online synopsis of the topic which shows the executive summary and key contacts sections. To view the full document, please download it.
| Topic title | Self-harm (2019) |
|---|---|
| Topic owner | Nottinghamshire and Nottingham City Suicide Prevention Steering Group |
| Topic author(s) | Jane O'Brien |
| Topic quality reviewed | August 2018 |
| Topic endorsed by | Nottinghamshire and Nottingham City Suicide Prevention Steering Group |
| Topic approved by | Health and Wellbeing Board March 2019 |
| Current version | March 2019 |
| Linked JSNA topics |
Executive summary
Download an accessible version of this infographic
Introduction
Within this all ages Self-harm Joint Strategic Needs Assessment (JSNA) chapter the Public Health England Fingertips Health Profile definition is used i.e.
Self-harm is defined as an intentional act of self-poisoning or self-injury irrespective of the type of motivation or degree of suicidal intent.
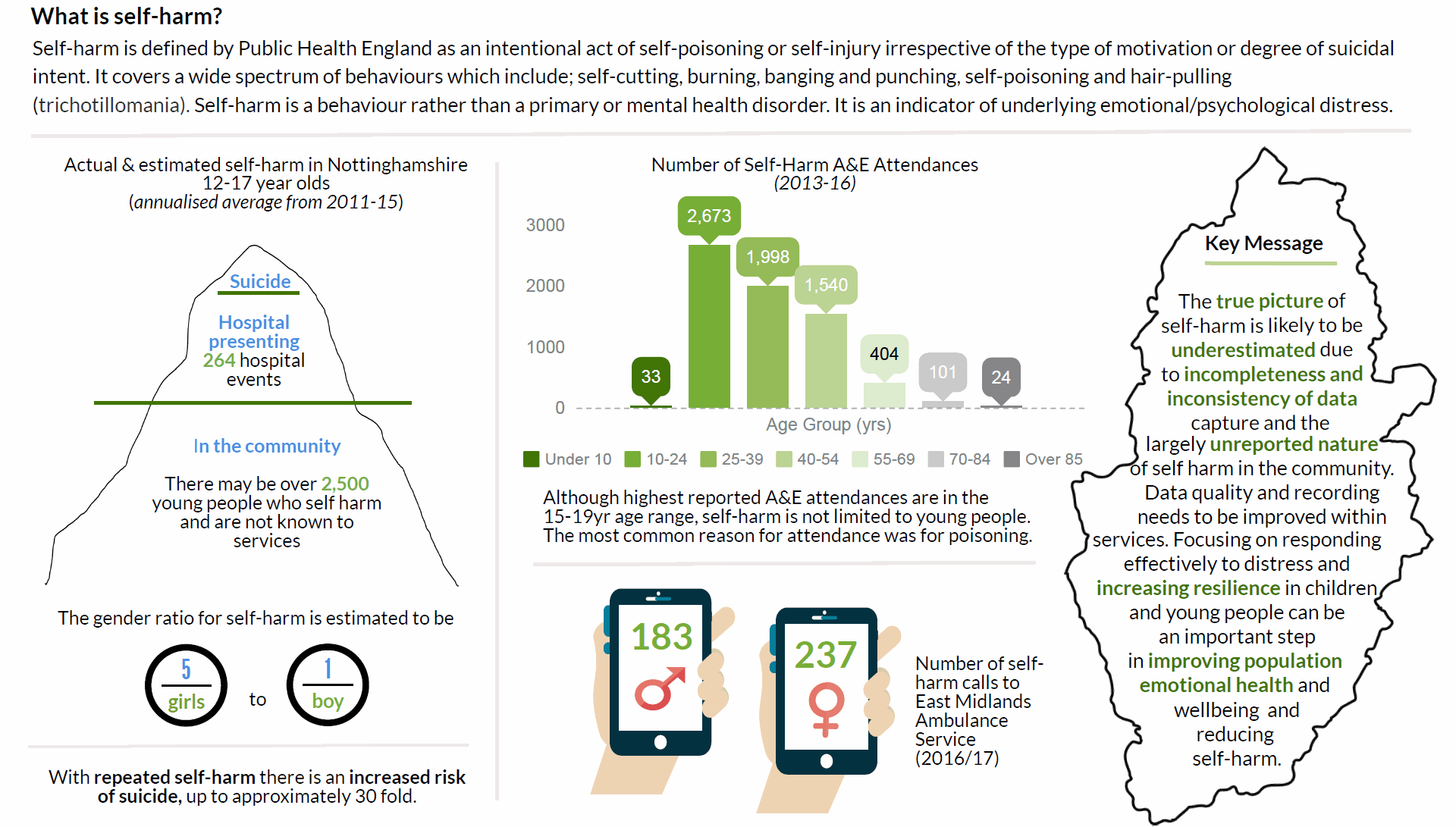
Self-harm is a behaviour rather than a primary or mental health disorder. It is an indicator of underlying emotional/psychological distress. Self-harm is not necessarily a suicide attempt, it may be a coping mechanism for dealing with intolerable situations. It is more common in children and young people with an estimated prevalence in the UK of between 1 in 12 and 1 in 15 between ages 11 and 25 years. Research shows that the incidence of self-harm in childhood and adolescence has increased in recent years with an increase of 68% in girls aged 13 to 16.
- The UK has the highest self-harm rate in young people of any country in Europe, with a rate of 400 per 100,000 population.
- Self-harm is more common in females than males with a girl to boy ratio of as much as 5 or 6 to 1 between ages 12 to 15 years.
- 22% of 15 year olds reported that they had self-harmed (32% of girls and 11% of boys) in surveys.
- Self-harm results in approximately 100,000 admissions to hospital a year (all ages) in England, 99% of which are emergency admissions
- Those that self-harm have a 1 in 6 chance of repeat emergency department (ED) attendance.
- People who repeat self-harm are at greater (up to approx. 30 fold) risk of suicide.
Self-harm is not limited to children and young people. The analysis in this JSNA chapter gives an indication of the size of the issue in the Nottinghamshire adult population based on numbers who have accessed clinical services and include;
- Between 2011 to 2015, approximately 220 young people between the ages of 12 to 17 years were recorded as actual self-harm hospital events and an estimated 2597 of self-harm in the community
- Between 2013 and 2016, Nottinghamshire Healthcare Foundation Trust recorded 2,141 self-harm adult referrals
- Between 2013 and 2016, self-harm A&E attendances was 6,788 between the ages 10 to 85 years.
The true picture of local needs is likely to be underestimated due to the incompleteness and inconsistency of data and the largely unreported nature of self-harm in the community.
This JSNA explores a range of risk factors contributing to self-harm, analysis of a range of service activity and referral data to estimate the size of the issue locally, evidence of what works from clinical guidance and lived experience of individuals and families.
Unmet need and gaps
Service and knowledge gaps are discussed in-depth in sections 8 and 9. The key themes underpinning the recommendations are:
Promotion, prevention and early intervention gaps
- There is a gap in non-clinical support and prevention, to address the root causes of self-harm.
- NICE guidelines and pathways begin when self-harm has been identified. The prevention element (CG16) focuses on prevention of re-occurrence. There are no system-wide support pathway/s that include health promotion, prevention and early intervention to help to reduce the initial occurrence of self-harm.
- There is a need to ensure continuing Public Health influence in the ICS Mental Health and Social Care Strategy work streams responsible for delivery of Pillar 2: Increasing Support for Prevention, Self-care and the Wider Determinants of Health and Pillar 3 Implementing a Person-centred Approach to Physical and Mental Health of the Draft Nottingham and Nottinghamshire STP All-age Integrated Mental Health and Social Care Strategy, particularly focusing on Adverse Childhood Experiences (ACE) and trauma informed practice.
- The true picture of local needs relating to promotion, prevention and early intervention is difficult to assess due to the incompleteness of data and largely unreported nature of self-harm.
- There is a gap in support for people of all ages who self-harm or who are at risk of self-harm, but do not meet acceptance criteria for clinical/mental health services.
Treatment and recovery gaps
- The majority of local data used in this document has come from commissioned treatment services and the main knowledge gaps relate to the incompleteness and inconsistency of the data.
- Self-harm is not limited to young people: analysis of hospital statistics shows a significant proportion of adults known to self-harm with a potential unknown proportion across all ages who do not access services or seek support.
Recommendations for consideration by commissioners
| Promotion, prevention and early intervention | Lead | |
|---|---|---|
| 1 |
Focus on reducing emotional distress/increasing resilience in children and young people, building on evaluation of current resilience programmes in schools. |
ICS Mental Health and Social Care Strategy Pillar 2 work stream |
| 2 |
Develop trauma/ACE informed practice across the health, care and education system and youth services. |
ICS Mental Health and Social Care Strategy Pillar 3 work stream |
| 3 |
Promote a community assets approach to support improved population emotional health and wellbeing, reduce social isolation and other underlying causes of self-harm across the life-course. |
Public Health |
| Treatment and recovery | ||
| 4 |
Improve data quality and recording in commissioned services to more specifically reflect self-harm and gain a better understanding of self-harm across all ages. This would enable a clearer assessment of need to inform development of interventions for promotion, prevention, early intervention, treatment and recovery. |
Clinical Commissioning Groups |
| 5 |
Develop system wide multi-agency (all ages) co-ordinated pathway/s recognising self-harm as a primary presenting need. |
Clinical Commissioning Groups |
Key contacts
This is an online synopsis of the topic which shows the executive summary and key contacts sections. To view the full document, please download it.